PrEP plays a fundamental role in helping to prevent new HIV diagnoses, but is underutilized1,2
PrEP is highly effective for preventing HIV1
According to the CDC, PrEP (pre-exposure prophylaxis) can reduce the chance of contracting HIV from sex by ~99% when taken as prescribed.
After 40 years of progress in reducing new HIV diagnoses, HIV remains a public health focus3
Only
36%

of the 1.2M people indicated for PrEP in 2022
were prescribed a PrEP medication2
(CDC, 2022 US estimates for individuals aged ≥16 years)
Groups most impacted by HIV continue to have low rates of PrEP use
Disparity by:
Black and Latine people
Black/African Americans represent
38%
of new HIV diagnoses4
(CDC, 2023. Estimated HIV diagnoses in the US and 6 territories and free states for individuals aged ≥13 years)
Latine people represent
34%
of new HIV diagnoses4
(CDC, 2023. Estimated HIV diagnoses in the US and 6 territories and free states for individuals aged ≥13 years)
In a retrospective analysis of PrEP prescriptions, Black and Latine people were disproportionately underprescribed PrEP relative to their need for HIV prevention.5



Actor portrayals.
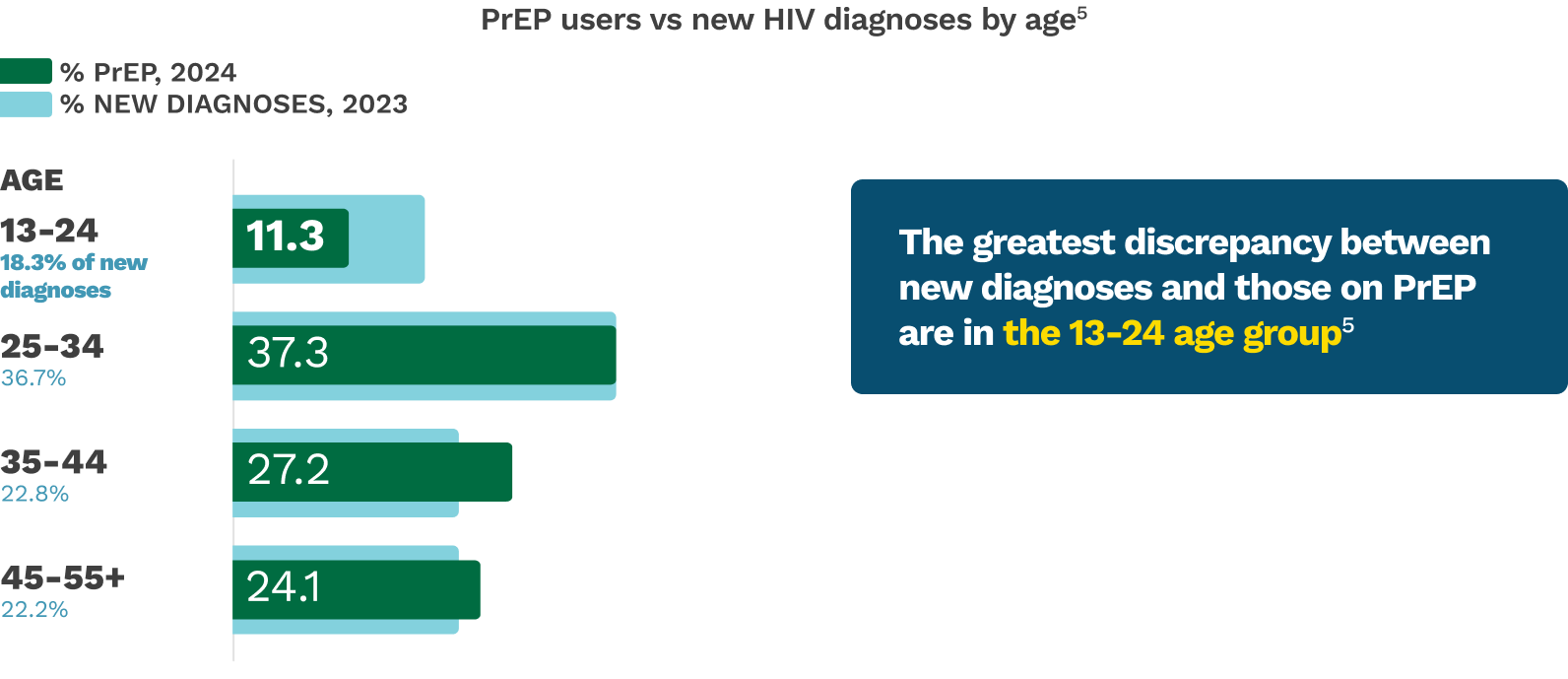
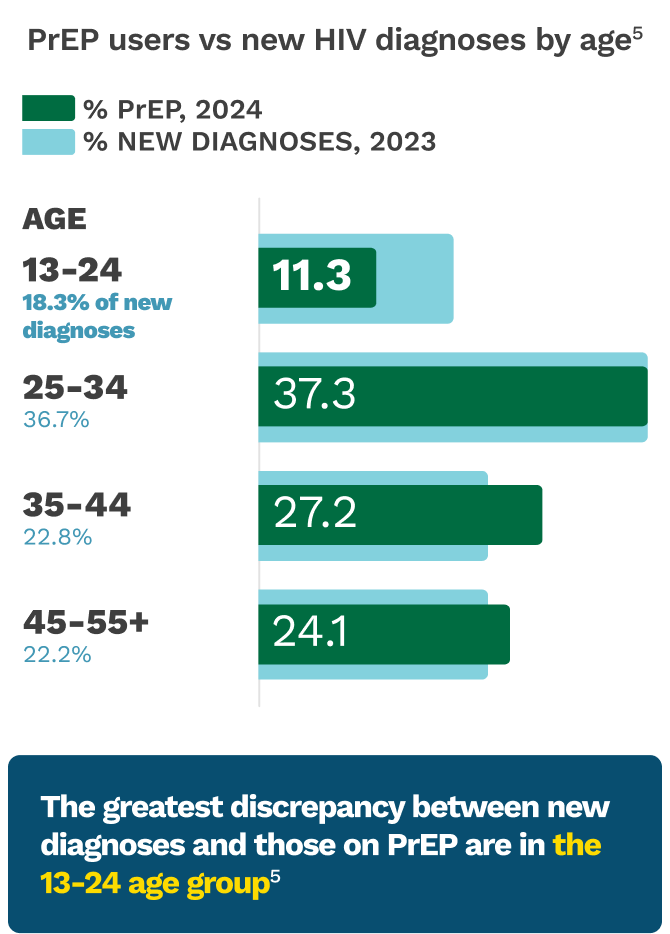
Young people
Young people aged 13-34 accounted for
Young people aged 13-34 accounted for
55%
of new HIV
diagnoses
in 20234
(CDC, 2023. Estimated HIV diagnoses in the US and 6 territories and free states for individuals aged ≥13 years)
2024 data showed that adolescents and young adults had the greatest unmet need for PrEP among all age groups.5

Actor portrayals.
Transgender women (TGW)
A meta-analysis of 98 studies showed:
TGW are 66x
more likely to be living with HIV
vs other individuals (aged >15 years)6
(Stutterheim SE, et al; 2021; N=48,604)
A 2019-2020 study showed low PrEP uptake:
32%
of HIV-negative
TGW
(n=288/902)
were on a PrEP medication7*
(CDC, National HIV Behavioral Surveillance report in 7 US cities)
*Took PrEP at any point in the 12 months before the interview to reduce the risk of getting HIV.7
Despite high awareness of PrEP, many TGW are concerned about PrEP interactions with gender-affirming hormone therapy (GAHT)7,8
In pharmacokinetic studies, there were
no clinically significant drug interactions impacting the levels of oral PrEP or GAHT when coadministered9-11
Consider BMD when choosing or prescribing PrEP
High prevalence of low bone mass
was observed in studies of TGW prior to/during GAHT, when compared with men as a reference point, according to DHHS12
In a 2020 Italian cross-sectional study that evaluated fracture risk in 57 TGW on estrogen replacement therapy after gender-confirming surgery
1 out of 7
showed an intermediate-high 10-year fracture risk8,13â€
†Participants (≥18 years old) were recruited from Turin, Italy, from January 2012 to May 2018.13

Actor portrayals.
See other considerations for TGWCloseKeep groups most impacted by HIV top of mind for HIV prevention conversations.
BMD=bone mineral density; CDC=Centers for Disease Control and Prevention; DHHS=US Department of Health and Human Services; GAHT=gender-affirming hormone therapy; Latine=a person of Latin American heritage; MSM=men who have sex with men; TGW=transgender women (who have sex with men).